Borderline personality disorder (or BPD) is a diagnosis that often carries with it both controversy and confusion. BPD isn’t all one thing or another and tv shows (like Crazy Ex-Girlfriend) and movies (such as Rachel Getting Married or Eternal Sunshine of the Spotless Mind) sometimes inadvertently add to the stigma of the diagnosis for some but may help to validate the diagnosis for others.
But men and women with a diagnosis of BPD can be the exact opposite of what is sometimes portrayed in the media. They may be smart, engaging, loyal, compassionate, and painfully self-aware.
Can you diagnose yourself with BPD?
The short answer is both yes and no. There are pros and cons to self-diagnosis as well as being diagnosed by therapists, social workers, psychologists, and psychiatrists.
Yes, you can diagnose yourself with BPD.
As a DBT therapist, many clients call me or come to my office having researched borderline personality disorder and believe that they meet diagnostic criteria (as defined by the American Psychiatric Association’s DSM-5) for BPD. Almost 100% of the time, my assessment concurs with their self-diagnosis.
I’m a huge fan of clients who have read about borderline personality disorder as a way to understand themselves and the diagnosis. I believe that well-educated clients who are proactive in getting treatment have an greater chance at feeling better sooner.
We could also argue that you are the expert in your own experience—not someone you just met. You might conclude: Who knows you better than you?
No, you cannot diagnose yourself with BPD.
We could also make the case that it’s better if you can have a diagnosis made by a licensed mental health professional who is able—over many sessions—to make an in-depth assessment using a variety of tools. This will include an interview where you’ll be asked lots of questions.
The symptoms of BPD often overlap with such diagnoses of bipolar disorder, ADHD, OCD, depression, and anxiety. People with BPD may also share characteristics of several other personality disorders such as narcissistic personality disorder, histrionic personality disorder, avoidant personality disorder, and schizotypal personality disorder.
Because people can have multiple diagnoses, it may be important to have an independent psychological evaluation completed by someone with extensive training and experience. This individual may be in a position to help you to understand your diagnosis and assist you in making some decisions about your next steps in treatment. Understanding those options may be more challenging when you are diagnosing yourself.
You are a unique person—not a diagnosis.
Finally, it may also be true that diagnoses (or “labels”) are not helpful for many people to understand themselves.
Your identification doesn’t have to come from a diagnosis. People aren’t “borderline” but they may have a diagnosis of borderline personality disorder. We would never tell someone, “You’re just a diabetic.” How we nonjudgmentally describe ourselves matters to us and it matters to others.
Many individuals decide to only focus on ways in which they can feel better, improve their ability to cope with difficult emotions, create healthier relationships, and achieve important academic or vocational goals. We can make the argument that a diagnosis of BPD (or any other mental health diagnosis) isn’t important at all—wellness or recovery is the ultimate goal.
Please don’t let a diagnosis define you or your future.
Recommendations for Learning More about BPD
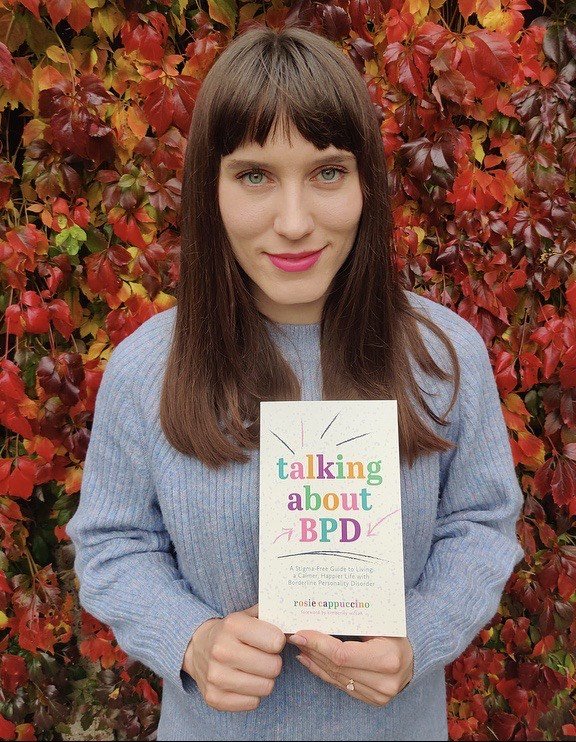
If you want to learn more about borderline personality disorder, I can strongly recommend checking out these books:
• Borderline Personality Disorder: A Guide for the Newly Diagnosed
• Beyond Borderline: True Stories of Recovery
• The Borderline Personality Disorder Wellness Planner for Families
You may also be interested in reading:
• How to Recover from Borderline Personality Disorder
• Treating Borderline Personality Disorder without Medications
• How to Let BPD Ruin Your Life
Interested in learning more about getting a diagnosis of borderline personality disorder or understanding your treatment options? Click here to learn more about my practice.